Source: Covexit
In the beginning of this fall season, everything points at an increasing number of outbreaks, infections, sick residents and deaths from COVID-19 in Canada’s elderly homes. Yes, there are measures that have been taken at the level of institutions offering care to the elderly but, with the growing number of outbreaks, these are already proving to be insufficient. The missing aspects in all the policies and measures seen so far are prophylaxis and early treatment. Experiences in France, the US, Australia and elsewhere suggest that at least 50% of deaths due to COVID-19 in nursing homes could be avoided. The treatments are extremely cheap and safe. They can not only be administered to nursing home residents but also to the caregivers, nurses and other personnel who are very exposed to the virus and are also at risk. This article contends that the extent of the anticipated bloodshed in nursing homes, in Canada and actually in other countries also denying treatment to the elderly, could to a large extent be contained through cheap and easy to implement therapies to be given to the elderly.
This is the end of the summer in Canada, which has the peculiar characteristic of having a very short fall season, and then there is a long winter – about 6 months from November to end of April.
Mon pays, ce n’est pas un pays, c’est l’hiver – My country, it’s not a country, it’s winter – said legendary singer Gilles Vigneault about the Province of Québec. This can be said for most of Canada, as only British Columbia has a somewhat less harsh climate.
Why start this article with such a platitude about Canada? Because there is a seasonality element with COVID-19, and currently a recurrence of the virus not only in the general population, but also in elderly homes.
In Canada, during the first phase of the pandemic, 81% of deaths occurred in elderly homes, either publicly or privately owned.
In Québec, the province with the highest death toll, out of 5 792 deaths attributed to COVID-19, nearly 5 000 occurred in elderly homes. Most if not all these elderly people who died were not hospitalized.
Reducing mortality from COVID-19 in Canada requires reducing mortality in the elderly homes.
In Ontario, as of September 25, there are 33 reported ongoing outbreaks in long-term care homes, and 25 outbreaks in retirement homes. The number of outbreaks is increasing: +4 in 2 days in long term care homes, and +3 in 2 days in retirement homes.
In Québec, as of September 25, there are 60 infected residents in 21 public elderly homes (CHSLD), 201 infected residents in 60 private nursing homes. Out of the 81 elderly homes where COVID-19 is present, five have over 25% of residents infected. These numbers are increasing on a daily basis.
In Alberta, as of Sept 24, there are 3 outbreaks in Acute care facilities, 4 in Long term care facilities and 12 in Supportive living/home living sites, i.e. a total of 22 outbreaks. No details are provided on this public website.
In British Columbia, there are 15 active outbreaks in care facilities (acute/long term/independent living), as of Sept 17.
Here is a more vivid account of what is happening, in a nursing home from the national capital’s area.
“As of Friday, 52 residents and 26 staff members have been infected with COVID-19 at West End Villa since an outbreak was declared there less than a month ago. Nine residents have now died, leaving families reeling. The death toll has gone up steadily in the past week and dozens more residents and staff members are awaiting test results.” reports a September 20 article.
This is not an isolated case, and this is just the beginning, very unfortunately. There are no reasons to believe the virus will not spread further in elderly homes in the coming months, even if various measures have been taken by provincial governments to attempt containing this spread.
Failed Public Health Policies Continued
When one is sick, it’s normal to seek and get treatment, especially in a country like Canada that claims to offer universal health care.
It’s also very normal to seek treatment early. Think about cancer for example. Everything is done to detect cancer early, as the chances of recovery are much higher when cancer treatment is started early.
This basic logic has unfortunately been little adopted when it comes to COVID-19. Not everywhere, but in many countries, including in Canada, the message of public health authorities has been for those testing positive to stay home, to self-isolate, and not to receive any medical attention until hospitalized.
The official policy was to seek medical help only when symptoms, such respiratory difficulties, were becoming unbearable. This could be after 7, 10 or more days of symptoms, providing ample time to the virus to replicate and induce a severe form of the disease.
Those with strong immune systems, typically younger people, would overcome the disease. Others would not, leading to hospitalization, sometimes transfer to the ICU, sometimes death.
Most of those getting COVID-19 in nursing homes were not hospitalized. There were numerous deaths not only linked to the viral infection, but also the lack of appropriate general care.
Many residents were left unfed, dehydrated. The staff, also left unprotected from virus, without any form of prophylaxis, and often missing PPE, often quit their job, or got sick themselves.
There were numerous outbreaks in nursing homes, some with very high death tolls and horrific conditions in which the elderly patients died.
Among the residences with the highest death tolls: in Quebec, in the vicinity of the Trudeau International Airport in Montreal, there were 51 deaths at the Herron CHLSD public elderly residence; in Ontario, at the Eatonville Care Centre, in the Toronto area, there were 42 deaths attributed to COVID-19.
With the collapse of the elderly care system, the Canadian army was asked to help. We previously wrote about the observational reports by the Canadian army about the situation in nursing homes, in Québec and Ontario.
It’s an horrible episode of Canadian history – but unfortunately, it may well reproduce itself in the coming months, as nothing fundamental has changed in the government’s policies towards elderly homes.
The situation is expected to be worsened by shortages of personnel. In Québec, 1700 nurses have already quit their job during the pandemic.
In Ontario, the Services Employees International Union Healthcare union says nearly 30 per cent or 7,500 of the nurses and personal support workers they represent have left their jobs or are planning on leaving.
The large infection rates and the deaths among health care workers are among the causes for the exodus from the health care professions.
In Ontario, over 6000 health care workers tested positive and 9 died. In nursing homes, in Ontario, a key union says 2,683 health care workers in long-term care homes have contracted the virus since March. In Québec, 14,000 health care workers tested positive and 3 died. There were no deaths among health care workers in other provinces, yet significant number of infections occurred in BC, Alberta and Nova Scotia.
No information is available about the long term health issues associated with infections among health care workers. Many are expected to be long haulers, having to endure long term side effects, in addition to the trauma associated with this horrific episode.
The Overwhelming Case for Treating Early in Elderly Homes
Totally absent from Canada’s federal and provincial strategies to fight COVID-19 in nursing homes, and actually also in the general population, is early treatment.
Early treatment requires a therapeutic intervention within days following COVID-19 first symptoms. Such intervention has been pioneered early in the pandemic. As we covered extensively in this blog, the concept is very simple: it’s to curb the replication of the virus early, to avoid a further development of the disease, reduce the need for hospitalization, the need for ICU transfer, and the number of deaths. Such an approach also reduces the likelihood of lasting symptoms, that are sometimes severe and can substantially ruin life quality for several years. These latter COVID-19 patients are often referred to as “long-haulers”.
It must be emphasized that the likelihood of developing a severe form of the disease, and the likelihood of death, grow exponentially with age.
A recent study by Professor Sir David Spiegelhalter about COVID-19 fatality rates in the UK, as a function of age, confirms that the disease mostly affects the elderly. What is remarkable is the near perfect logarithmic relationship between age and fatality.
The study indicates that the risk doubles every 5.75 years. To give some examples from the study, the number of deaths from COVID-19 per 100,000 inhabitants was 0.5 for those aged 15 to 24, 4.9 for those aged 35 to 44, 49.5 for those aged 55 to 64, 461 for those aged 75 to 84 and 2040 for those aged 90 or more.
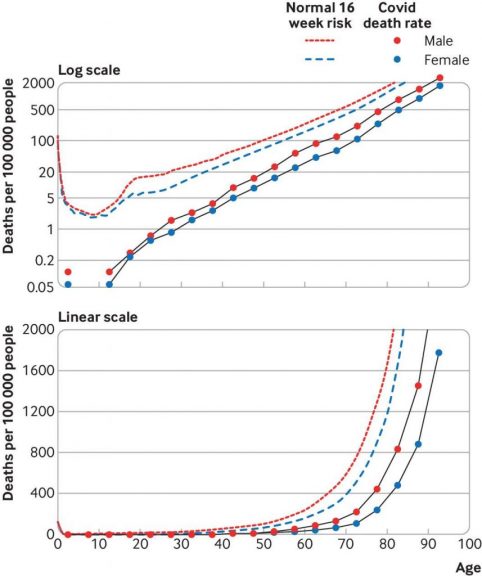
Another way to look at those numbers: 1 out 211 780 died from COVID-19 among those aged 15 to 24, while 1 out of 90 died from those aged 85 to 89.
And let’s keep in mind, the UK, like Canada, denied any form of early treatment to the population, so there is likely similarity in the link between age and mortality.
In Canada, the elderly, especially in nursing homes, have not been seen as worth receiving much therapeutic efforts to save them from COVID-19. This meant they were left dying in the nursing homes, mostly without any attempted treatment.
And here is the fundamental flaw: such treatments exist, are extremely safe, can save numerous lives, and yet they are being denied to the elderly. They are also denied to the health care workers, who are among the highest risks segments of society.
Money-wise, these treatments are extremely cheap – less than $50 -, and actually would generate colossal savings to the health care system, by reducing the likelihood of large outbreaks and of crisis situations in elderly homes, as experienced this past spring.
Unfortunately, Canada has not been alone in denying early treatment to nursing home residents. There are very few studies about the use of such early treatments for seniors, but they are some, and they clearly indicate the suitability of such treatments to reduce lethality.
On June 9, an article by Pirnay et al, titled “Beneficial effect of the hydroxychloroquine/ azithromycin combination in elderly patients with COVID-19: Results of an observational study,” was published on ScienceDirect. The article has been accepted, peer reviewed and awaits for publication in the journal “Le Pharmacien Hospitalier et Clinicien.”
This was a study on 68 elderly patients, all having tested COVID-19 positive through a PCR test, with an average age of 86.2 years – 25% male. Over 50% of those patients presented with comorbidities.
The provided treatment was 600 mg of hydroxychloroquine per day for 10 days and azithromycin for 5 days (500 mg on the first day and 250 mg on each of the following days). No zinc supplement was provided. There was ECG monitoring and anticoagulants were also given to patients.
The authors recognize it’s a small study that was conducted in a crisis situation, yet stress the short time frame – median of 2.5 days, average of 4.4 days – between the apparition of symptoms and the start of the HCQ/AZT treatment led to a favorable outcome.
During the study period, 7 out of the 68 patients studied died. All deaths occurred due to severe respiratory complications of the disease. The remaining patients were considered cured after clinical signs disappeared within 21 days after the PCR positive test.
The authors conclude that the HCQ/AZT association provides real benefits for a majority of elderly patients.
The observed lethality rate of 10% needs to be put into the context of lethality rates observed during the pandemic in elderly homes in France, which was around 27%.
On August 18, Professor Didier Raoult reported on unpublished work by IHU-Marseille in elderly homes. He indicates that the lethality rate in these nursing homes, without early treatment, was about 27% in France, according to official data.
Professor Raoult also reported the outcomes of a therapeutic intervention that was done in a Marseille elderly home, where the lethality rate without treatment was 27.8% while it was 14.4% with the HCQ/AZT treatment.
This brought Professor Raoult to declare that 50% of the deaths attributed to COVID-19 in elderly homes in France could have been avoided, would his early treatment protocol had been implemented on a large scale in France’s nursing homes.
What seems clear from these therapeutic interventions with elderly patients is that the lethality rate can be dramatically reduced. Achieving at least a 50% reduction appears to be very realistic, on the basis of these French experiences.
It’s important to stress that early treatment protocols involving zinc, such as the Zelenko protocol, may be even more efficient. To be noted is that the Zelenko protocol, also relying on HCQ and AZT, uses lower dose HCQ, for a shorter period of time, than the typical HCQ/AZT protocol used in France.
A timely administration of the therapy, at first symptoms, is also critical. This was emphasized by Watanabe, when analyzing data from a clinical trial with hydroxychloroquine only, which is a much less effective treatment than the tri-therapies that are now recommended by Professor Borody, Dr Zelenko and others. The shorter the treatment starts after exposure to the virus, the better are the therapeutic outcomes.

In the study by Pirnay et al, the administration of the drug took place, in average, 4.4 days after the first symptoms, which can clearly be improved upon. In an elderly home setting, this could easily be brought to within 1 or 2 days after the first symptoms, if the proper processes are implemented, and this can be expected to further reduce the lethality rate.
It’s important to emphasize that, in addition to reducing lethality, curing many elderly from COVID-19 will allow them continue their life, and ultimately move towards death, in dignity, surrounded by their family, and not in the horrific conditions that have happened this past Spring.
Actually, while elderly residents are the most vulnerable in nursing homes, one should not forget about the health care workers and other personnel, who are likely to be exposed to the virus.
Early treatment of such workers, in case of symptoms and positive tests, is also essential, not only to contain the development of the disease, and possibly avoid long term sequels or death, but also to reduce contagion and transmission to non-infected residents or other health care workers.
There is also a strong case for such health care workers to receive prophylaxis, to avoid developing a severe form of the disease. While there is now a variety of prophylaxis protocols available, we will not review them in this article.
Actually, before any positive COVID-19 test, because of the high risk of propagation of the virus in nursing homes, prophylaxis could also be offered to residents, either in a strong form (with hydroxychloroquine or ivermectin), or in a softer form, with supplements only: quercetin, zinc, vitamins c and d.
It’s worth pointing out here to the experience at The Resort nursing home in Texas City, where the attending GP, Dr Robin Armstrong, was pro-active and treated all the infected residents hydroxychloroquine, azithromycin and zinc (Zelenko protocol).
The treatment protocol he describes in his interview with The Texan news outlet is: hydroxychloroquine: 400 mg twice a day on day 1, 200 mg twice a day on days 2 to 5; azithromycin 500 mg on day 1, and 250 mg on days 2 to 5; zinc: 250 mg once a day for all 5 days. “That was it: 5 day regiment” says Dr Armstrong.
Dr Armstrong recorded only 1 death out of 38 treated patients. There was another death, of a lady who was aged 102, but she died after having recovered from COVID-19, according to Dr Armstrong. Without treatment, Dr Armstrong expected to lose 15 to 20% of the residents to COVID-19.
What Dr Armstrong also emphasizes is that, thanks to the early treatment, except for one, the infected staff recovered quickly from the disease and returned to work within days. Accordingly, treating early infected staff is important not only for their health and prompt recovery, but also to avoid havoc in the management and the orderly provision of care of the nursing homes.
Finally, it’s important to note that reducing lethality in nursing homes, as well as reducing contagion and the size of the outbreaks with early treatment, will lead to much less traumatic experiences for health care workers. As already indicated, many of them are now leaving their career, because of the risks, the trauma and crazy hours they were asked to perform.
Consequently, early treatment of the elderly infected with COVID-19 would play a key role in keeping those health care workers in their profession.
Perspectives of Two World-Class Experts
Our most recent interviews featured two world-class experts: Professor Thomas Borody from Australia and Professor Christian Perronne from France. Both answer specific questions about how to best treat the elderly. Both recommend to treat, not to let patients go without treatment. Both recommend treating early the elderly patients having contracted COVID-19. It should be common sense and mainstream knowledge, but it’s not, even if it is already known for 6 months or so.
Here are some excerpts of the interview of Professor Thomas Borody.
“The therapy we are talking about is more than Ivermectin, but it’s Ivermectin, Doxycycline and Zinc… We treat patients for 10 days, with Ivermectin in the appropriate dosage, and Doxycycline daily and Zinc daily. They all actually have activity against the intra-cellular multiplication of the virus. … It’s just hard to believe how simple it is to cure coronavirus.”
“There is no age limit in treating. In effect, it has been used without any major side effect in the treatment of pregnant women and children. We don’t recommend they should. But it works fairly well in elderly people. Remember, elderly people also have elderly immune systems. So it takes much longer for the swabs to become negative.”
“You can treat virtually at any age. We have examples of people who just turned the corner in their 60s to 70s, in 3 or 4 days, as far as in their 90s, and people improve. The attending GP treats the patient. It works in the elderly as well as any other group.”
And here are excerpts of our interview with Professor Christian Perronne.
Q: What is your solution to manage an outbreak in an elderly home?
“For me, they should have a stockpile of hydroxychloroquine, azithromycin and maybe zinc. They should also have diagnostic tests. If there are one or two cases, they should diagnose all the other residents of the nursing home. They should try to isolate positive patients from the others. Possibly, if there is an extension of the epidemic inside the institution, the institution should possibly provide prophylactic hydroxychloroquine. We know now from several studies in the world that it works. Of course, they should treat the cases immediately.”
“During the epidemic wave in March and April in France, in some nursing homes for elderly people, in some institutions, there were 30%, sometimes 50%, of the residents who died. I know an institution in the center of Paris where many elderly people died. The nurses didn’t want to come back to work. Some had COVID-19. Some were afraid. The elderly people were abandoned … When the authorities came to the clinic, the elderly people could not go out. Some were completely dehydrated. Some were dead in their bed for several days. It was horrible. This was in the center of Paris. Imagine in other countries, everywhere in the world, I think it happened also.”
“The GPs are now authorized to prescribe. In many nursing homes for elderly people, they sometimes don’t have full time physicians. There are GPs coming part time to take care of the residents. Probably, they could prescribe with a private prescription. I hope so. The directors of these institutions could try to obtain a stockpile. Normally, there is not [ legal ] text that forbids that.”
Q: Can the families of the elderly put pressure for early treatment to be provided?
“Of course, the families could play a major role for advocacy to help the residents. I received many many letters from families, who were very shocked by the way their parents or grand-parents were treated in these institutions. In France, the population is very upset by what happened. I hope that it won’t come back… If there were a second wave, we should be able to treat it freely. All the French physicians ask to be free to prescribe, according to their experience, the literature, and not to be driven by the government’s so stupid decisions that led to the death of thousands of people.”

The Time to Implement Early Treatment in Elderly Homes is NOW
While not hit first by the pandemic, Canada was ill-prepared to deal with the COVID-19 outbreaks in elderly homes. There was a bloodshed in elderly homes, with 81% out of the 9,000 deaths that occurred in the country.
In this month of September, there are already new outbreaks, and the measures that have been decided in the provinces all neglect to use what is probably the most important and effective tool to save lives and limit the scope of the outbreaks: early treatment.
it’s very reasonable to believe that at least 50% of new COVID deaths in elderly homes could be avoided by using early therapies, which are extremely safe, extremely cheap and extremely simple to administer.
Actually, elderly homes, as with the constant presence of nursing personnel, are an ideal place to detect infections and to administer treatments very early, within one or two days after the first symptoms. Ideally, testing needs to take place before, but treatment should not be delayed in case of delays in testing – as treating early is extremely important, especially with elderly patients with weak immune systems.
How many lives could be saved in nursing homes in the coming months? Probably hundreds, if not thousands, in Canada alone. During the first wave, about 7,000 nursing home residents died. If we make the assumption that the new measures would reduce mortality, without treatment, by 50%, one could expect about 3,500 deaths from COVID-19. If treatment is given, this number could be divided by two, i.e. 1,750 lives could be saved.
Conversely, not treating, as currently decided by the federal and provincial authorities, means accepting a toll of 1,750 avoidable deaths, according to this scenario. The real numbers could be lower, or higher, maybe much higher. But the rule of thumb that not treating in a nursing home means incurring the double of the deaths that would occur with treatment is likely a realistic one, based on the experience in France and other “anecdotical evidence” as reported by Dr Robin Armstrong in Texas.
Medical doctors working in nursing homes have a critical role to play to administer such treatment. Even if there is no formal recommendation by the provincial or federal authorities for such treatments to be provided, medical doctors need to assert their right to prescribe. It is their responsibility to do what’s best for their patients. In this case, early treatment can in many cases make the difference between life and death, or at the very least between the absence or presence of long term symptoms.
Early treatment is not a compassionate, end of life, treatment. If one waits for the viral infection and for severe symptoms to develop, then the treatment does not work. The earliest the treatment is given after the first symptoms, the higher are the chances of a prompt full recovery – all the experts who know about early treatment agree on this.
The benefits of treating early COVID-19 positive elderly people would be considerable not only in terms of saved lives but also in terms of the health and safety of the personnel, which might be less enticed to quit the health care related professional careers because of the risks associated with COVID-19.
It is pretty absurd that early treatment is not top of the list of the guidelines dealing with COVID-19 in elderly homes. It’s pretty absurd, but it’s a reality.
And let’s not forget, the winter is long in Canada. Nursing homes are closed environments where the virus easily propagates. The virus will continue to have multiple opportunities to find its way in nursing homes and infect residents, whatever institution-level or governmental measures have been taken to attempt reducing infections.
Hopefully, the present analysis will bring medical doctors, the management of nursing homes, and the relevant authorities to adopt the common sense recommendation to treat early the elderly.
Families also have an important role to play, as they can at least demand for early treatment to be provided to their loved ones, who are the most vulnerable in our society, who are extremely afraid of what is coming in the coming months.
Elderly residents not only need, but also deserve, to be protected from COVID-19, and should not be left dying, without treatment, as in the first wave of the pandemic.
Post Script #1:
Those who think that a randomized controlled trial is needed before taking action may want to refer to Professor Thomas Borody’s comments about when such trials are justified:
“… uneducated brains would think that everything requires randomized controlled trials, but it doesn’t. There is a whole list of conditions where RCTs are inappropriate. So they should go back and read, and maybe do medicine all over again …”
Post Script #2:
Last April, the author of this article sent a detailed analysis to the Prime Minister of Québec, explaining how early treatment should be generalized as soon as possible in the province, to reduce lethality in the general population. He was not heard, and the Province went much further, by preventing medical doctors to offer such treatments, compromising the right to prescribe, and leading to numerous avoidable deaths. The summary of the proposal sent to Prime Minister Legault can be found here.
It’s most likely the present analysis and recommendation to treat early in elderly homes will also be disregarded, and that many additional avoidable deaths will occur. At least, the document will have been written. In case there are public enquiries into the new likely disaster in the making, hopefully, those preventing early treatment to occur will be held to account. That would be the minimum that society should expect when public health policy is carried out in such an irresponsible way, when human life is seen as expandable, when letting die elderly people from COVID-19. untreated, is seen as normal and not as criminal.
Related:
Belgium Study 8,075 patients: Low HCQ doses resulted in lower mortality in Covid patients
Chronic treatment with hydroxychloroquine and SARS-CoV-2 infection.
‘Hydroxychloroquine’ And The COVID-19 Political Battlefield. It Became 2020’s Dirty Word.

