Source: Science Direct
aLoghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
bIranian Research Center for HIV/AIDS, Iranian Institute for Reduction of High-Risk Behaviors, Tehran University of Medical Sciences, Tehran, Iran
cCenter for Communicable Disease Control (CDC), IHR National Focal Point, Ministry of Health & Medical Education, Tehran, Iran
dMinistry of Health and Medical Education, Tehran, Iran, AIDS/STI Control Dep. Ministry of Health and Medical Education, Eyvanak street, Shahrak-e-Gharb-Tehran, Iran
eMinistry of Health and Medical Education, Tehran Iran, Eyvanak street, Shahrak-e-Gharb Tehran, Iran
fHealth Service Management, Deputy of Health, Ministry of Health and Medical Education, Tehran, Iran
gMinistry of Health and Medical Education, Tehran Iran, Eyvanak street Shahrak-e-Gharb, Tehran, Iran
hResearch Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
iSchool of Medicine, Shiraz University of Medical Sciences, Shiraz Iran, Deputy of Health, Ministry of Health and Medical Education, Tehran, Iran
jDepartment of Pharmacotherapy, Tehran University of Medical Sciences, Tehran, Iran
kDepartment of Pharmacotherapy, Tehran University of Medical Sciences, Tehran, Iran Postal Code: 1417614411, P.O.Box: 14155/6451
Highlights
• Early administration of HCQ reduced the odds of hospitalization by 38%.
• Early administration of HCQ reduced the odds of death by 73%%.
• In resource-poor countries, HCQ may be still an option for mild COVID-19.
Abstract
The role of hydroxychloroquine (HCQ) in early outpatient management of mild coronavirus disease 2019 (COVID-19) needs further investigation.
This study was a multicenter, population-based national retrospective-cohort investigation of 28,759 adults with mild COVID-19 seen at the network of Comprehensive Healthcare Centers (CHC) between March and September 2020 throughout Iran. The baseline characteristics and outcome variables were extracted from the national integrated health system database.
A total of 7,295 (25.37%) patients who presented with mild COVID-19 within 3 to 7 days of symptoms onset received HCQ (400 mg twice daily on day 1 followed by 200 mg twice daily for the next four days and were then followed for 14 days).
The main outcome measures were hospitalization or death for six months follow-up. COVID-19-related hospitalizations or deaths occurred in 523 (7.17%) and 27 (0.37%) respectively, in HCQ recipients and 2,382 (11.10%) and 287 (1.34%) respectively, in non-recipients. The odds of hospitalization or death was reduced by 38% (odds ratio [OR] = 0.62; 95% confidence interval [CI]: 0.56–0.68, p = < 0.001) and 73% (OR = 0.27; 95% CI: 0.18–0.41, p = < 0.001) in HCQ recipients and non-recipients.
These effects were maintained after adjusting for age, comorbidities, and diagnostic modality. No serious HCQ-related adverse drug reactions were reported.
In our large outpatient national cohort of adults with mild COVID-19 disease who were given HCQ early in the course of the disease, the odds of hospitalization or death was reduced significantly regardless of age or comorbidities.
1. Introduction
Since the start of human transmission of Severe Acute Respiratory Coronavirus-2 (SARS CoV-2) to date (February 5, 2021), the virus has claimed 2,265,354 out of 104,165,006 confirmed cases globally.[1] Despite experiencing a year of the pandemic and the development and deployment of multiple vaccines, efforts to find effective treatment with outcome benefits in patients with coronavirus disease 2019 (COVID-19) have remained futile.
Hydroxychloroquine (HCQ) was one of the first medications that were repurposed for the treatment of COVID-19. Following the publication of in-vitro and non-randomized clinical studies, [2], [3] HCQ use rapidly increased to the extent that it was prescribed for about 60% of hospitalized patients with COVID-19 in the United States in March 2020.3 This level decreased to 12% in May 2020 owing to the ineffectiveness of HCQ as shown in subsequent studies. [4], [5] Nevertheless, the controversy concerning its efficacy continued until randomized clinical trials (RCTs), such as the randomized evaluation of COVID-19 therapy (RECOVERY) and Solidarity trials confirmed the lack of efficacy of HCQ in hospitalized patients with COVID-19. [6], [7]
Currently, most guidelines, such as those from the National Institutes Health (NIH) and infectious diseases society of America (IDSA), recommend against the use of HCQ for hospitalized patients. [8], [9] Besides, from the early onset of its use, there was a concern about a potential property of HCQ in QTc interval prolongation as demonstrated on electrocardiography (ECG) tracings, particularly in patients with a history of cardiovascular diseases. Some studies have shown an increased in the risk of arrhythmias and ECG abnormalities following administration of HCQ, especially in combination with azithromycin. [10], [11], [12]
However, with the publication of subsequent studies, this concern has been somewhat alleviated. [6], [13], [14] Taken together, these factors once again led to attention being paid to HCQ use in outpatient settings.
The first confirmed case of COVID-19 in Iran was diagnosed on February 18, 2020. [15] A scientific COVID-19 taskforce was promptly assembled by the Iranian Ministry of Health (MOH) and five days later, the first national protocol for the management of the COVID-19 in outpatient settings was developed.
On February 29, 2020, the responsibility for providing outpatient services to the COVID-19 patients across a vast span of communities in Iran was assigned to the Comprehensive Health Centers (CHCs). The extensive CHC network of 5,500 centers is the main provider of primary healthcare in Iran. These centers work free of charge in 16- or 24-h rosters and cover both rural and urban populations. These centers are governed by their regional medical science universities and health services authorities under the jurisdiction of the MOH throughout the whole country. [16] The health information of more than 90% of the population in Iran is registered in an electronic network of health records that are maintained by these centers. Allocation of these CHCs to function as the main body for primary care, data collection, and registration centers for COVID-19 facilitates the screening and follow-up of these patients, especially in the high-risk populations.
In this large population-based study, we evaluated the clinical outcomes of mild COVID-19 patients who were treated with HCQ in an outpatient setting.
2. Methods
In this outpatient national retrospective cohort study, the clinical outcomes of patients with mild COVID-19 were followed in two main groups of patients who received or did not receive HCQ.
HCQ was added to the supportive care for patients with mild COVID-19 illness who did not require referral to the hospital. Based on the national COVID-19 protocol, the mild disease was defined as the presence of mild cough, body ache, loss of smell or taste, a body temperature of ≤ 38 °C, peripheral oxygen saturation (SpO2) ≥ 93%, and the absence of shortness of breath, altered hemodynamics, and mental status instability.
HCQ was provided to the patients who presented with no clear contraindications and were not using it for other indications. They were instructed to take 400 mg twice daily on day 1 followed by 200 mg twice daily from days 2 to 5 if they had presented within 3 to 7 days of the initiation of their COVID-19 symptoms.
Patients were followed daily for 5 days and then on day 14, either in-person or by phone, for their disease trajectory, outcome variables, and adverse HCQ-related drug reactions. Baseline characteristics and outcome variables of hospitalization or death for all patients were also collected from the national integrated health system database.
COVID-19 was diagnosed based on the clinical presentation and either reverse transcriptase-polymerase chain reaction (RT-PCR) results from nasopharyngeal swab samples following World Health Organization (WHO) protocols or chest imaging. The clinical outcomes of our study were COVID-19-related hospitalizations or deaths during six-months of follow up.
Continuous and categorical variables are shown as mean ± standard deviation (SD) and frequency (percentage), respectively. OR and 95% CI were estimated for comparison of outcomes of the patients who were treated or not treated with HCQ by binary logistic regression models. The effect of confounding variables, including age, sex, body mass index (BMI), hypertension, respiratory diseases, diabetes mellitus, and cardiovascular diseases, other than hypertension, on the incidence of outcomes was examined by adjusted logistic regression models. The selection of these factors was based on their effects on the clinical outcomes of the patients with mild to moderate COVID-19 as described in previous studies.[18]
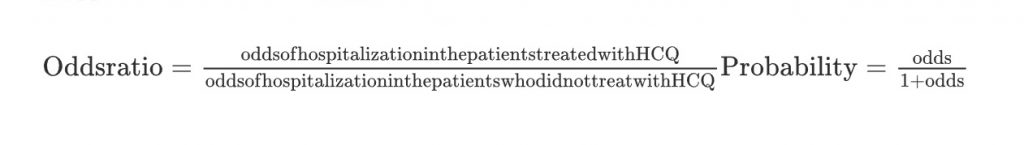
To calculate cost saving of HCQ administration, the probability of hospitalization was estimated using following formulas:
3. Results
From March 2020 to September 2020, the COVID-19 related data concerning a total of 28,759 patients who presented to the CHCs were included in the integrated health system for final analysis. COVID-19 diagnosis was made by clinical parameters and RT-PCR in 22,784 (79.22%) and clinical parameters and chest imaging in the remaining patients (Table 1). Upon presentation, evaluation, and a brief education about COVID-19 and possible HCQ adverse reaction, a total of 7,295 (25.37%) patients with mild symptoms consented to receive and use HCQ as prescribed.
Table 1. Baseline characteristics and clinical outcomes of the patients who received and did not receive hydroxychloroquine
| Variable | Received HCQ (N=7,295) | Did not receive HCQ(N=21,464) | OR (95% CI) | P- Value |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Median age (IQR) – yr | 43 (33-57) | 43 (33-58) | – | 0.112 |
| Age category – no. (%) | ||||
| ≤65 yr | 6,424 (88.06) | 18,557 (86.45) | – | 0.001 |
| >65 to ≤85 yr | 825 (11.31) | 2,710 (12.63) | – | |
| >85 yr | 46 (0.63) | 197 (0.92) | – | |
| Sex – no. (%) | ||||
| Male | 3,674 (50.36) | 10,924 (50.89) | – | 0.220 |
| Female | 3,621 (49.64) | 10,540 (49.11) | – | |
| COVID-19 risk factors – no. (%) | ||||
| Without risk | 4,724 (64,76) | 14,365 (66.93) | – | <0.001 |
| With at least 1 risk | 2,571 (35.24) | 7,099 (33.07) | – | |
| Hypertension | 1,023 (14.02) | 2,864 (13.34) | – | 0.074 |
| Respiratory diseases | 636 (8.72) | 1,782 (8.30) | – | 0.140 |
| Diabetes mellitus | 426 (5.84) | 982 (4.58) | – | <0.001 |
| Non-hypertensive cardiovascular diseases | 308 (4.22) | 907 (4.23) | – | 0.508 |
| Obesity (BMI >30 kg/m2) | 122 (1.67) | 415 (1.93) | – | 0.085 |
| History of corticosteroid use | 110 (1.51) | 281 (1.31) | – | 0.114 |
| Malignancy | 43 (0.59) | 126 (0.59) | – | 0.526 |
| Cancer therapy | 32 (0.44) | 98 (0.46) | – | 0.462 |
| Organ transplant recipient | 14 (0.19) | 33 (0.15) | – | 0.292 |
| HIV positive | 9 (0.12) | 21 (0.10) | – | 0.344 |
| COVID-19 diagnosis – no. (%) | ||||
| PCR positive | 5,964 (81.76) | 16,820 (78.36) | – | <0.001 |
| PCR negative | 470 (6.44) | 1,418 (6.61) | – | |
| No test | 861 (11.80) | 3,226 (15.03) | – | |
| Clinical outcomes – no. (%) | ||||
| Hospitalization (unadjusted) | 523 (7.17) | 2,382 (11.10) | 0.62 (0.56-0.68) | <0.001 |
| Hospitalization (adjusted*) | – | – | 0.62 (0.56-0.69) | <0.001 |
| Death (unadjusted) | 27 (0.37) | 287 (1.34) | 0.27 (0.18-0.41) | <0.001 |
| Death (adjusted*) | – | – | 0.30 (0.20-0.45) | <0.001 |
| Hospitalization in patients with positive PCR | 408 (6.84) | 1,598 (9.50) | 0.70 (0.63-0.78) | <0.001 |
| Hospitalization in patients with negative PCR | 24 (5.11) | 154 (10.86) | 0.44 (0.28-0.69) | <0.001 |
| Hospitalization in patients with no test | 91 (10.57) | 630 (19.53) | 0.49 (0.39-0.62) | <0.001 |
| Death in patients with positive PCR | 18 (0.30) | 151 (0.90) | 0.33 (0.21-0.55) | <0.001 |
| Death in patients with negative PCR | 1 (0.21) | 4 (0.28) | 0.75 (0.08-6.76) | 0.801 |
| Death in patients with no test | 8 (0.93) | 132 (4.09) | 0.22 (0.11-0.45) | <0.001 |
The mean age ± SD of the patients was 45 ± 15 and 46 ± 15 years old in those who received and did not receive HCQ, respectively. No significant gender differences in both groups were noted (Table 1). Hypertension, chronic respiratory diseases, and diabetes mellitus were the most common underlying reported diseases. Hospitalization for COVID-19 worsening was required in 7.17% and 11.1% of patients who received and did not receive HCQ, respectively. HCQ reduced the odds of hospitalization by 38% (OR=0.62; 95% CI: 0.56–0.68, p-value=< 0.001).
A total of 314 patients died of COVID-19 complications, 27 (0.37%) and 287 (1.34%) in those who receive and did not receive HCQ respectively, indicating a 73% mortality risk reduction on logistic regression model (OR = 0.27; 95% CI: 0.18–0.41, p ≤ 0.001) in the HCQ group.
The effect of HCQ on the outcome measures was maintained after adjusting for confounding factors and comorbidities. This effect remained significant whether patients were diagnosed based on positive RT-PCR or otherwise (Table 1).
According to the odds of hospitalization of patients who received (0.077) or did not receive (0.124) HCQ, the probability of this outcome was 0.07 and 0.11 respectively. Dividing the difference of these numbers by 0.11 it was estimated that hospitalization costs were reduced by about 36 percent.
Serious HCQ adverse drug reactions were not reported in any of the age groups with or without comorbidities.
4. Discussion
In this large national retrospective cohort study, we examined the clinical outcomes of the patients with mild COVID-19 following early treatment with HCQ in an outpatient setting. Our study demonstrated that a short course of HCQ, given in the outpatient setting and within seven days of symptoms, could significantly reduce hospitalizations and deaths. The odds of COVID-19-related hospitalizations and deaths in our study population who were treated with HCQ were reduced by more than one-third and two-thirds, respectively.
In our study, we included the effects of confounding factors on the occurrence of outcome measures and recorded any serious HCQ adverse reactions.
In the light of severe and prolonged burden caused by SARS-CoV-2, the importance of its early detection and management, and the lack of an effective, available, and cheap therapeutic option, our study along with others [19], [20], [21] may convey important messages regarding the outpatient management of mild COVID-19 disease.
In Iran, the mean direct medical cost for each hospitalized patient with COVID-19 was estimated to be 59,203,409 Rials (approximately $ 3,755). [22] Administration of HCQ can reduce the hospitalization cost by about 36 percent. Assuming a population of 100 patients, the total costs of hospitalization are calculated as $ 41,305 (11× 3,755) without administration of HCQ while this cost will decrease to $ 26,285 (7× 3,755) with considering the medication. Of course, if indirect costs are also considered, the effect of HCQ will be far greater. It should be noted that mean indirect cost of each patient with COVID-19 was estimated as $ 11,634. [22]
The impact of triple therapy, including HCQ, azithromycin, and zinc on hospitalization rates and all-cause deaths was examined in a retrospective study. The dose of HCQ was 200 mg twice daily for five days in that study. Use of the triple regimen caused a significant reduction in the incidence rates of hospitalization and all-cause mortality (OR = 0.16 and 0.2, respectively). [19] Although this study was also retrospective, the number of included patients was much smaller than found in our study. In this study, concomitant medications, and adverse effects of HCQ were mentioned. The patients were risk-stratified based on age, symptoms, and comorbidities.
The impact of medications, such as HCQ, prednisolone, azithromycin, ivermectin, and oseltamivir on clinical outcomes of 717 COVID-19 patients was examined retrospectively in an outpatient setting in Brazil. The main outcomes of the study were the rates of hospitalization and deaths as in our study. The use of HCQ alone was associated with 55% reduction in the rate of hospitalization. While not significant, the same decrease was seen with respect to the incidence of death. Except for prednisolone, other medications had no significant effect on the outcomes. [20] Interestingly, cardiac and ECG abnormalities were not seen in any of the above studies. [19], [20]
Beneficial effects of HCQ in outpatient were also described in a systematic review. [23] Currently, several random clinical trials (RCTs) are ongoing with the aim of evaluating the efficacy of HCQ, specifically in COVID-19 disease outpatient management. [24], [25]
However, two recent RCTs for early HCQ use in non-hospitalized patients did not indicate any significant association with a reduction in the risk of hospitalization. [26], [27]
Several studies especially RCTs demonstrated that HCQ can be administrated safely and without incidence of serious cardiac adverse events in outpatients and hospitalized patients with mild COVID-19. [14], [28], [29], [30]
Some of the limitations of our study are the retrospective design, lack of laboratory data (as the patients were deemed to be mild and not followed for hospital laboratory values), lack of access to other medications received by the patients in each group, absence of data on patients who required hospital admission, and a short initial follow-up period.
However, our large, multicenter, national study and adjustment of the outcome variables for comorbidities are the strengths of our study.
5. Conclusion
Our investigation of a large national cohort appears to support early administration (within the first 3 to 7 days of COVID-19 diagnosis) of HCQ in mild COVID-19 disease in an outpatient setting for reducing hospitalizations and deaths without any serious adverse HCQ-related effects.
If this finding is confirmed in future clinical trials, HCQ as a cheap and available drug may still play a role in a specific population with respect to reducing COVID-19 burden, particularly in resource-poor countries.
Uncited reference
[17].
Acknowledgment
Data were extracted from CHCs affiliated to following Medical Sciences Universities. We appreciate all staffs for data gathering and sharing.
Abadan University of Medical Sciences, Arak University of Medical Sciences, Ardabil University of Medical Sciences, Urmia University of Medical Sciences, Hamedan University of Medical Sciences (Asadabad branch), North Khorasan University of Medical Sciences (Esfarayen branch), Isfahan University of Medical Sciences, Alborz University of Medical Sciences, Iran University of Medical Sciences, Zahedan University of Medical Sciences (Iranshahr), Ilam University of Medical Sciences, Babol University of Medical Sciences, North Khorasan University of Medical Sciences (Bojnourd branch), Kerman North Khorasan University of Medical Sciences (Bam branch), Hormozgan University of Medical Sciences, Ahwaz Jundishapur University of Medical Sciences (Bahbahan branch), Bushehr University of Medical Sciences, Birjand University of Medical Sciences, Tabriz University of Medical Sciences, Mashhad University of Medical Sciences (Torbat Jam branch), Tehran University of Medical Sciences, Jahrom University of Medical Sciences, Jiroft University of Medical Sciences, Ardabil University of Medical Sciences (Khalkhal branch), Khomein University of Medical Sciences, Urmia University of Medical Sciences (Khoy branch), Dezful University of Medical Sciences, Rafsanjan University of Medical Sciences, Zabol University of Medical Sciences, Zanjan University of Medical Sciences, Mazandaran University of Medical Sciences, Saveh University of Medical Sciences, Sabzevar University of Medical Sciences, Tabriz University of Medical Sciences (Sarab branch), Semnan University of Medical Sciences, Sirjan University of Medical Sciences, Shahrood University of Medical Sciences, Shahrekord University of Medical Sciences, Shahid Beheshti University of Medical Sciences, Ahwaz Jundishapur University of Medical Sciences (Shushtar branch), Shiraz University of Medical Sciences, Fasa University of Medical Sciences, Qazvin University of Medical Sciences, Qom University of Medical Sciences, Kashan University of Medical Sciences, Kordestan University of Medical Sciences, Gonabad University of Medical Sciences, Gilan University of Medical Sciences, Shiraz University of Medical Sciences (Larestan branch), Lorestan University of Medical Sciences, Maragheh University of Medical Sciences, Neyshabur University of Medical Sciences, Yasuj University of Medical Sciences, Yazd University of Medical Sciences
We would like to thank the nurses and other staffs of Imam Khomeini Hospital Complex for their kind supports and also Ms. Ava Khalili for English proofreading the manuscript.
Funding
The authors did not receive any fund for this work.
References
[1]WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/. Accessed on February 5, 2021.Google Scholar
[2]X. Yao, F. Ye, M. Zhang, C. Cui, B. Huang, P. Niu, X. Liu, L. Zhao, E. Dong, C. Song, S. Zhan, R. Lu, H. Li, W. Tan, D. LiuIn Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)Clin Infect Dis., 71 (15) (2020 Jul 28), pp. 732-739, 10.1093/cid/ciaa237CrossRefView Record in ScopusGoogle Scholar
[3]P. Gautret, J.C. Lagier, P. Parola, V.T. Hoang, L. Meddeb, M. Mailhe, B. Doudier, J. Courjon, V. Giordanengo, V.E. Vieira, H. Tissot Dupont, S. Honoré, P. Colson, E. Chabrière, B. La Scola, J.M. Rolain, P. Brouqui, D. RaoultHydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trialInt J Antimicrob Agents., 56 (1) (2020 Jul), Article 105949, 10.1016/j.ijantimicag.2020.105949ArticleDownload PDFView Record in ScopusGoogle Scholar
[4]C.J. Clancy, M.H. NguyenA first draft of the history of treating coronavirus disease 2019 (COVID-19): Use of repurposed medications in United States hospitalsOpen Forum Infectious Diseases. (2020 Dec 15), 10.1093/ofid/ofaa617Google Scholar[5]J. Geleris, Y. Sun, J. Platt, J. Zucker, M. Baldwin, G. Hripcsak, A. Labella, D.K. Manson, C. Kubin, R.G. Barr, M.E. Sobieszczyk, N.W. SchlugerObservational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19N Engl J Med., 382 (25) (2020 Jun 18), pp. 2411-2418, 10.1056/NEJMoa2012410CrossRefView Record in ScopusGoogle Scholar
[6]RECOVERY Collaborative Group, Horby P, Mafham M, Linsell L, Bell JL, Staplin N, Emberson JR, Wiselka M, Ustianowski A, Elmahi E, Prudon B, Whitehouse T, Felton T, Williams J, Faccenda J, Underwood J, Baillie JK, Chappell LC, Faust SN, Jaki T, Jeffery K, Lim WS, Montgomery A, Rowan K, Tarning J, Watson JA, White NJ, Juszczak E, Haynes R, Landray MJ. Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19. N Engl J Med. 2020 Nov 19;383(21):2030-2040. doi: 10.1056/NEJMoa2022926Google Scholar
[7]WHO Solidarity Trial Consortium, Pan H, Peto R, Henao-Restrepo AM, Preziosi MP, Sathiyamoorthy V, Abdool Karim Q, Alejandria MM, Hernández García C, Kieny MP, Malekzadeh R, Murthy S, Reddy KS, Roses Periago M, Abi Hanna P, Ader F, Al-Bader AM, Alhasawi A, Allum E, Alotaibi A, Alvarez-Moreno CA, Appadoo S, Asiri A, Aukrust P, Barratt-Due A, Bellani S, Branca M, Cappel-Porter HBC, Cerrato N, Chow TS, Como N, Eustace J, García PJ, Godbole S, Gotuzzo E, Griskevicius L, Hamra R, Hassan M, Hassany M, Hutton D, Irmansyah I, Jancoriene L, Kirwan J, Kumar S, Lennon P, Lopardo G, Lydon P, Magrini N, Maguire T, Manevska S, Manuel O, McGinty S, Medina MT, Mesa Rubio ML, Miranda-Montoya MC, Nel J, Nunes EP, Perola M, Portolés A, Rasmin MR, Raza A, Rees H, Reges PPS, Rogers CA, Salami K, Salvadori MI, Sinani N, Sterne JAC, Stevanovikj M, Tacconelli E, Tikkinen KAO, Trelle S, Zaid H, Røttingen JA, Swaminathan S. Repurposed Antiviral Drugs for Covid-19 – Interim WHO Solidarity Trial Results. N Engl J Med. 2020 Dec 2. doi: 10.1056/NEJMoa2023184.Google Scholar
[8]COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment guidelines. National Institutes of Health. Available at https://www.covid19treatmentguidelines.nih.gov/. Updated on 9 Oct 2020. Accessed on 16 Dec 2020.Google Scholar
[9]A. Bhimraj, R.L. Morgan, A.H. Shumaker, V. Lavergne, L. Baden, et al.Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19Clin Infect Dis., ciaa478 (2020), p. 2020, 10.1093/cid/ciaa478Updated on 20 AugGoogle Scholar
[10]E.S. Rosenberg, E.M. Dufort, T. Udo, L.A. Wilberschied, J. Kumar, J. Tesoriero, P. Weinberg, J. Kirkwood, A. Muse, J. DeHovitz, D.S. Blog, B. Hutton, D.R. Holtgrave, H.A. ZuckerAssociation of Treatment with Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York StateJAMA., 323 (24) (2020 Jun 23), pp. 2493-2502, 10.1001/jama.2020.8630CrossRefView Record in ScopusGoogle Scholar
[11]F. Bessière, H. Roccia, A. Delinière, R. Charrière, P. Chevalier, L. Argaud, M. CourAssessment of QT Intervals in a Case Series of Patients With Coronavirus Disease 2019 (COVID-19) Infection Treated With Hydroxychloroquine Alone or in Combination With Azithromycin in an Intensive Care UnitJAMA Cardiol., 5 (9) (2020 Sep 1), pp. 1067-1069, 10.1001/jamacardio.2020.1787CrossRefView Record in ScopusGoogle Scholar
[12]N.J. Mercuro, C.F. Yen, D.J. Shim, T.R. Maher, C.M. McCoy, P.J. Zimetbaum, H.S. GoldRisk of QT Interval Prolongation Associated With Use of Hydroxychloroquine With or Without Concomitant Azithromycin Among Hospitalized Patients Testing Positive for Coronavirus Disease 2019 (COVID-19)JAMA Cardiol., 5 (9) (2020 Sep 1), pp. 1036-1041, 10.1001/jamacardio.2020.1834CrossRefView Record in ScopusGoogle Scholar
[13]Self WH, Semler MW, Leither LM, Casey JD, Angus DC, Brower RG, Chang SY, Collins SP, Eppensteiner JC, Filbin MR, Files DC, Gibbs KW, Ginde AA, Gong MN, Harrell FE Jr, Hayden DL, Hough CL, Johnson NJ, Khan A, Lindsell CJ, Matthay MA, Moss M, Park PK, Rice TW, Robinson BRH, Schoenfeld DA, Shapiro NI, Steingrub JS, Ulysse CA, Weissman A, Yealy DM, Thompson BT, Brown SM; National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, Steingrub J, Smithline H, Tiru B, Tidswell M, Kozikowski L, Thornton-Thompson S, De Souza L, Hou P, Baron R, Massaro A, Aisiku I, Fredenburgh L, Seethala R, Johnsky L, Riker R, Seder D, May T, Baumann M, Eldridge A, Lord C, Shapiro N, Talmor D, O’Mara T, Kirk C, Harrison K, Kurt L, Schermerhorn M, Banner-Goodspeed V, Boyle K, Dubosh N, Filbin M, Hibbert K, Parry B, Lavin-Parsons K, Pulido N, Lilley B, Lodenstein C, Margolin J, Brait K, Jones A, Galbraith J, Peacock R, Nandi U, Wachs T, Matthay M, Liu K, Kangelaris K, Wang R, Calfee C, Yee K, Hendey G, Chang S, Lim G, Qadir N, Tam A, Beutler R, Levitt J, Wilson J, Rogers A, Vojnik R, Roque J, Albertson T, Chenoweth J, Adams J, Pearson S, Juarez M, Almasri E, Fayed M, Hughes A, Hillard S, Huebinger R, Wang H, Vidales E, Patel B, Ginde A, Moss M, Baduashvili A, McKeehan J, Finck L, Higgins C, Howell M, Douglas I, Haukoos J, Hiller T, Lyle C, Cupelo A, Caruso E, Camacho C, Gravitz S, Finigan J, Griesmer C, Park P, Hyzy R, Nelson K, McDonough K, Olbrich N, Williams M, Kapoor R, Nash J, Willig M, Ford H, Gardner-Gray J, Ramesh M, Moses M, Ng Gong M, Aboodi M, Asghar A, Amosu O, Torres M, Kaur S, Chen JT, Hope A, Lopez B, Rosales K, Young You J, Mosier J, Hypes C, Natt B, Borg B, Salvagio Campbell E, Hite RD, Hudock K, Cresie A, Alhasan F, Gomez-Arroyo J, Duggal A, Mehkri O, Hastings A, Sahoo D, Abi Fadel F, Gole S, Shaner V, Wimer A, Meli Y, King A, Terndrup T, Exline M, Pannu S, Robart E, Karow S, Hough C, Robinson B, Johnson N, Henning D, Campo M, Gundel S, Seghal S, Katsandres S, Dean S, Khan A, Krol O, Jouzestani M, Huynh P, Weissman A, Yealy D, Scholl D, Adams P, McVerry B, Huang D, Angus D, Schooler J, Moore S, Files C, Miller C, Gibbs K, LaRose M, Flores L, Koehler L, Morse C, Sanders J, Langford C, Nanney K, MdalaGausi M, Yeboah P, Morris P, Sturgill J, Seif S, Cassity E, Dhar S, de Wit M, Mason J, Goodwin A, Hall G, Grady A, Chamberlain A, Brown S, Bledsoe J, Leither L, Peltan I, Starr N, Fergus M, Aston V, Montgomery Q, Smith R, Merrill M, Brown K, Armbruster B, Harris E, Middleton E, Paine R, Johnson S, Barrios M, Eppensteiner J, Limkakeng A, McGowan L, Porter T, Bouffler A, Leahy JC, deBoisblanc B, Lammi M, Happel K, Lauto P, Self W, Casey J, Semler M, Collins S, Harrell F, Lindsell C, Rice T, Stubblefield W, Gray C, Johnson J, Roth M, Hays M, Torr D, Zakaria A, Schoenfeld D, Thompson T, Hayden D, Ringwood N, Oldmixon C, Ulysse C, Morse R, Muzikansky A, Fitzgerald L, Whitaker S, Lagakos A, Brower R, Reineck L, Aggarwal N, Bienstock K, Freemer M, Maclawiw M, Weinmann G, Morrison L, Gillespie M, Kryscio R, Brodie D, Zareba W, Rompalo A, Boeckh M, Parsons P, Christie J, Hall J, Horton N, Zoloth L, Dickert N, Diercks D. Effect of Hydroxychloroquine on Clinical Status at 14 Days in Hospitalized Patients With COVID-19: A Randomized Clinical Trial. JAMA. 2020 Dec 1;324(21):2165-2176. doi: 10.1001/jama.2020.22240.Google Scholar
[14]A. Mohana, T. Sulaiman, N. Mahmoud, M. Hassanein, A. Alfaifi, E. Alenazi, N. Radwan, N. AlKhalifah, E. Elkady, A. Almohaizeie, F. AboGazalah, K. AlabdulKareem, F. AlGhofaili, H. Jokhdar, F. AlrabiahHydroxychloroquine safety outcome with an approved therapeutic protocol for COVID-19 outpatients in Saudi ArabiaInt J Infect Dis., 17 (102) (2020 Oct), pp. 110-114, 10.1016/j.ijid.2020.10.031Google Scholar
[15]M. Jalili, P. Payandemehr, A. Saghaei, H.N. Sari, H. Safikhani, P. KolivandCharacteristics and Mortality of Hospitalized Patients With COVID-19 in Iran: A National Retrospective Cohort StudyAnn Intern Med., 20 (2020 Jul), pp. M20-2911, 10.7326/M20-2911View Record in ScopusGoogle Scholar
[16]A. Raeisi, J.S. Tabrizi, M.M. GouyaIR of Iran National Mobilization against COVID-19 EpidemicArch Iran Med., 23 (4) (2020 Apr 1), pp. 216-219, 10.34172/aim.2020.01CrossRefView Record in ScopusGoogle Scholar
[17]National guidance of diagnosis and treatment of COVID-19 in both inpatient and outpatients setting. https://medcare.behdasht.gov.ir/. Updated on 13 Dec 2020. Accessed on 19 Dec 2020.Google Scholar
[18]R.T. Gandhi, J.B. Lynch, C. Del RioMild or Moderate Covid-19N Engl J Med., 383 (18) (2020 Oct 29), pp. 1757-1766, 10.1056/NEJMcp2009249CrossRefView Record in ScopusGoogle Scholar
[19]R. Derwand, M. Scholz, V. ZelenkoCOVID-19 outpatients: early risk-stratified treatment with zinc plus low-dose hydroxychloroquine and azithromycin: a retrospective case series studyInt J Antimicrob Agents., 56 (6) (2020 Dec), Article 106214, 10.1016/j.ijantimicag.2020.106214ArticleDownload PDFView Record in ScopusGoogle Scholar[20]S.N. Szente Fonseca, Sousa A de Queiroz, A.G. Wolkoff, M.S. Moreira, B.C. Pinto, C.F. Valente Takeda, E. Rebouças, A.P. Vasconcellos Abdon, A.L.A. Nascimento, H.A. RischRisk of hospitalization for Covid-19 outpatients treated with various drug regimens in Brazil: Comparative analysisTravel Med Infect Dis., 31 (38) (2020 Oct), Article 101906, 10.1016/j.tmaid.2020.101906ArticleDownload PDFView Record in ScopusGoogle Scholar
[21]Ip A, Ahn J, Zhou Y, Goy AH, Hansen E, Pecora AL, Sinclaire BA, Bednarz U, Marafelias M, Mathura S, Sawczuk IS, Underwood III JP, Walker DM, Prasad R, Sweeney RL, Ponce MG, LaCapra S, Cunningham FJ, Calise AG, Pulver BL, Ruocco D, Mojares GE, Eagan MP, Ziontz KL, Mastrokyriakos P, Goldberg SL. . Hydroxychloroquine in the treatment of outpatients with mildly symptomatic COVID-19: a multi-center observational study. medRxiv preprints 2020; August 25. https://doi.org/10.1101/2020.08.20.20178772.Google Scholar
[22]M. Ghaffari Darab, K. Keshavarz, E. Sadeghi, J. Shahmohamadi, Z. KavosiThe economic burden of coronavirus disease 2019 (COVID-19): evidence from IranBMC Health Serv Res., 21 (1) (2021 Feb 11), p. 132, 10.1186/s12913-021-06126-8View Record in ScopusGoogle Scholar
[23]C. Prodromos, T. RumschlagHydroxychloroquine is effective, and consistently so when provided early, for COVID-19: a systematic reviewNew Microbes New Infect., 38 (2020 Nov), Article 100776, 10.1016/j.nmni.2020.100776ArticleDownload PDFView Record in ScopusGoogle Scholar
[24]S. Göpel, W. Bethge, P. Martus, F. Kreth, T. Iftner, S. Joos, S. Döbele, B. Mordmüller, P. Kremsner, T. Ettrich, T. Seufferlein, M. Bitzer, N. MalekTest and treat COVID 65 plus – Hydroxychloroquine versus placebo in early ambulatory diagnosis and treatment of older patients with COVID19: A structured summary of a study protocol for a randomised controlled trialTrials., 21 (1) (2020 Jul 10), p. 635, 10.1186/s13063-020-04556-zView Record in ScopusGoogle Scholar
[25]Duvignaud A, Lhomme E, Pistone T, Onaisi R, Sitta R, Journot V, Nguyen D, Peiffer-Smadja N, Crémer A, Bouchet S, Darnaud T, Poitrenaud D, Piroth L, Binquet C, Michel JF, Lefèvre B, Lebeaux D, Lebel J, Dupouy J, Roussillon C, Gimbert A, Wittkop L, Thiébaut R, Orne-Gliemann J, Joseph JP, Richert L, Anglaret X, Malvy D; COVERAGE study group. Home Treatment of Older People with Symptomatic SARS-CoV-2 Infection (COVID-19): A structured Summary of a Study Protocol for a Multi-Arm Multi-Stage (MAMS) Randomized Trial to Evaluate the Efficacy and Tolerability of Several Experimental Treatments to Reduce the Risk of Hospitalisation or Death in outpatients aged 65 years or older (COVERAGE trial). Trials. 2020 Oct 13;21(1):846. doi: 10.1186/s13063-020-04619-1.Google Scholar
[26]Mitjà O, Corbacho-Monné M, Ubals M, Tebe C, Peñafiel J, Tobias A, Ballana E, Alemany A, Riera-Martí N, Pérez CA, Suñer C, Laporte P, Admella P, Mitjà J, Clua M, Bertran L, Sarquella M, Gavilán S, Ara J, Argimon JM, Casabona J, Cuatrecasas G, Cañadas P, Elizalde-Torrent A, Fabregat R, Farré M, Forcada A, Flores-Mateo G, Muntada E, Nadal N, Narejos S, Gil-Ortega AN, Prat N, Puig J, Quiñones C, Reyes-Ureña J, Ramírez-Viaplana F, Ruiz L, Riveira-Muñoz E, Sierra A, Velasco C, Vivanco-Hidalgo RM, Sentís A, G-Beiras C, Clotet B, Vall-Mayans M; BCN PEP-CoV-2 RESEARCH GROUP. Hydroxychloroquine for Early Treatment of Adults with Mild Covid-19: A Randomized-Controlled Trial. Clin Infect Dis. 2020 Jul 16:ciaa1009. doi: 10.1093/cid/ciaa1009.Google Scholar
[27]C.P. Skipper, K.A. Pastick, N.W. Engen, A.S. Bangdiwala, M. Abassi, S.M. Lofgren, D.A. Williams, E.C. Okafor, M.F. Pullen, M.R. Nicol, A.A. Nascene, K.H. Hullsiek, M.P. Cheng, D. Luke, S.A. Lother, L.J. MacKenzie, G. Drobot, L.E. Kelly, I.S. Schwartz, R. Zarychanski, E.G. McDonald, T.C. Lee, R. Rajasingham, D.R. BoulwareHydroxychloroquine in Nonhospitalized Adults With Early COVID-19: A Randomized TrialAnn Intern Med., 173 (8) (2020 Oct 20), pp. 623-631, 10.7326/M20-4207CrossRefView Record in ScopusGoogle Scholar
[28]S.M. Lofgren, M.R. Nicol, A.S. Bangdiwala, K.A. Pastick, E.C. Okafor, C.P. Skipper, M.F. Pullen, N.W. Engen, M. Abassi, D.A. Williams, A.A. Nascene, M.L. Axelrod, S.A. Lother, L.J. MacKenzie, G. Drobot, N. Marten, M.P. Cheng, R. Zarychanski, I.S. Schwartz, M. Silverman, Z. Chagla, L.E. Kelly, E.G. McDonald, T.C. Lee, K.H. Hullsiek, D.R. Boulware, R. RajasinghamSafety of Hydroxychloroquine Among Outpatient Clinical Trial Participants for COVID-19. Open ForumInfect Dis. (2020 Oct 19;7(11):ofaa500.), 10.1093/ofid/ofaa500Google Scholar
[29]Million M, Lagier JC, Gautret P, Colson P, Fournier PE, Amrane S, Hocquart M, Mailhe M, Esteves-Vieira V, Doudier B, Aubry C, Correard F, Giraud-Gatineau A, Roussel Y, Berenger C, Cassir N, Seng P, Zandotti C, Dhiver C, Ravaux I, Tomei C, Eldin C, Tissot-Dupont H, Honoré S, Stein A, Jacquier A, Deharo JC, Chabrière E, Levasseur A, Fenollar F, Rolain JM, Obadia Y, Brouqui P, Drancourt M, La Scola B, Parola P, Raoult D. Early treatment of COVID-19 patients with hydroxychloroquine and azithromycin: A retrospective analysis of 1061 cases in Marseille, France. Travel Med Infect Dis. 2020 May-Jun;35:101738. doi: 10.1016/j.tmaid.2020.101738.Google Scholar
[30]Lagier JC, Million M, Gautret P, Colson P, Cortaredona S, Giraud-Gatineau A, Honoré S, Gaubert JY, Fournier PE, Tissot-Dupont H, Chabrière E, Stein A, Deharo JC, Fenollar F, Rolain JM, Obadia Y, Jacquier A, La Scola B, Brouqui P, Drancourt M, Parola P, Raoult D; IHU COVID-19 Task force. Outcomes of 3,737 COVID-19 patients treated with hydroxychloroquine/azithromycin and other regimens in Marseille, France: A retrospective analysis. Travel Med Infect Dis. 2020 Jul-Aug;36:101791. doi: 10.1016/j.tmaid.2020.101791Google Scholar
Related: Journal of Medicine Says HCQ + Zinc Reduces COVID Deaths
This doctor cured 5000 corona patients with hydroxychloroquine
Timing and dosing are the key to HCQ + AZ treatment in elderly Covid-19 patients

